
A stroke, sometimes called a “brain attack,” occurs when the blood supply to a part of your brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. Without oxygen, brain cells can begin to die within minutes, leading to lasting brain damage, long-term disability, or even death.
There are three main types:
Ischaemic stroke: Caused by a blockage (like a blood clot) cutting off blood flow to the brain.
Haemorrhagic stroke: Caused by bleeding in or around the brain.
Transient ischaemic attack (TIA) – often called a mini-stroke, where the symptoms are temporary but still a warning sign

FAST TEST
If you ever suspect someone’s having a stroke, remember the F.A.S.T. test:
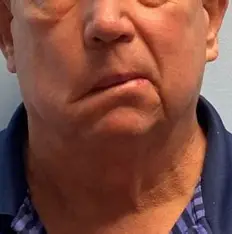
- Face: Can they smile? Has their face drooped?
- Arms: Can they lift both arms?
- Speech: Is their speech slurred or strange?
- Time: Time to call emergency services immediately.
Emergency Treatments
Surgery: For haemorrhagic strokes, surgery may be needed to relieve pressure on the brain or repair damaged blood vessels
Thrombolysis: A clot-busting drug like alteplase or tenecteplase is used to dissolve clots in ischaemic strokes. It must be given within 4.5 hours of symptom onset for best results.
Thrombectomy: A surgical procedure to physically remove a clot from a large artery in the brain. It’s most effective when done within hours of the stroke.


First Aid for Stroke
Try to remember when symptoms started—this helps doctors decide on treatment.
Use the F.A.S.T. test:
Face: Ask them to smile. Is one side drooping?
Arms: Can they raise both arms? Does one drift downward?
Speech: Is their speech slurred or strange?
Time: If you see any of these signs, call 999 immediately.
Call emergency services:
Dial 999 (or 112) and say you suspect a stroke. Time is critical—some treatments are only effective within a few hours.
Keep them calm and still:
Help them sit or lie down in a comfortable position.
If they’re conscious, reassure them that help is on the way.
Do not give them food or drink:
Swallowing may be impaired, increasing the risk of choking.
Monitor their condition:
Watch for changes in responsiveness or breathing.
If they become unresponsive and not breathing, begin CPR if trained.
Note the time: