
Hyperventilation
occurs when you breathe too fast and deeply, exhaling more than you inhale. This can cause symptoms like dizziness, chest pain, and shortness of breath. It often happens due to anxiety or stress, but can also be caused by medical conditions. When you hyperventilate, your body loses too much carbon dioxide, leading to narrowed blood vessels and reduced blood flow to the brain, making you feel lightheaded.
If it happens frequently, it may be a condition called hyperventilation syndrome.
Signs and Symtoms Of Hyperventilation
- Feeling anxious or panicked, hyperventilation is often linked to stress.
- Dizziness or lightheadedness – due to reduced blood flow to the brain.
- Shortness of breath – feeling like you can’t get enough air.
- Chest pain or tightness – often mistaken for heart-related issues.
- Rapid heartbeat – a pounding sensation in the chest.
- Tingling or numbness – especially in the hands, feet, or around the mouth.
- Muscle spasms – particularly in the hands and feet.
- Dry mouth and sweating are common.
Treatment: Hyperventilation
- Controlled Breathing: To regulate oxygen and carbon dioxide levels, encourage the casualty to take slow, deep breaths in through the nose and out through the mouth.
- Distraction Techniques: Progressive muscle relaxation and visualisation exercises can help calm your body and mind.
- Reassurance & Environment: Moving to a quiet space and reducing external stressors can help regain control of breathing.
- Medical Advice: If hyperventilation is frequent, consulting a healthcare professional is recommended to rule out underlying conditions.
- If casualty shows signs of hypoxia call 999/112

The casualty should not breathe into a paper bag or plastic bag if there is the possibility of a more serious underlying problem/condition that could make matters worse. i.e. Asthma
Drowning

Drowning has profound physiological effects on the body, primarily due to oxygen deprivation. Here’s what happens:
- Brain: The brain is the first organ to suffer from hypoxia (lack of oxygen). Brain cells begin dying within minutes, which can lead to permanent neurological damage if resuscitation is delayed.
- Heart: Initially, the heart may beat faster in response to stress, but as oxygen levels drop, it can become arrhythmic and eventually stop.
- Lungs: Water entering the lungs disrupts gas exchange, leading to inflammation and fluid buildup, which can cause acute respiratory distress syndrome (ARDS).
- Autonomic Responses: The body may experience cold shock, laryngospasm (airway closure), and electrolyte imbalances, all of which contribute to drowning-related complications.
Survivors of drowning incidents may suffer from long-term complications, including neurological impairment, lung infections, and Cardiac issues.
Secondary drowning
It is a rare but serious condition that occurs when water enters the lungs, leading to irritation and fluid buildup, known as pulmonary oedema. This can cause breathing difficulties that may worsen over the next 24 hours.
Changes in behaviour, such as irritability or low energy levels, which may indicate the brain isn’t getting enough oxygen
Persistent coughing
Chest pain
Trouble breathing
Extreme fatigue
Call 999/112 for Emergency Help!


Treatment For Drowning
- Call for Help – Alert emergency services immediately.
- Rescue Safely – Use a flotation device or extend an object to pull them to safety. Avoid putting yourself at risk.
- Check Responsiveness – If unconscious, lay them on their back and check for breathing.
- Perform CPR – If they are not breathing, start chest 30 compressions at a rate 100-120 per minute. If an AED is available, place pads on the casualty and listen to the instructions.
- Rescue Breaths – give 2 rescue breaths after every 30 compressions.
- Monitor for Vomiting – Be prepared to roll them onto their side to clear their airway if they vomit.
- Treat for Hypothermia – Cover them with warm clothes or blankets if needed.
If they regain consciousness, place them in the recovery position and continue monitoring until emergency help arrives.
Never enter water to rescue a drowning casualty unless you are trained and equipped. The water could be cold, deep, and have strong currents. Use rope, a stick/pole, or an object that will float, where possible.
STAY SAFE!
Sucking Chest wound/Collapsed Lung
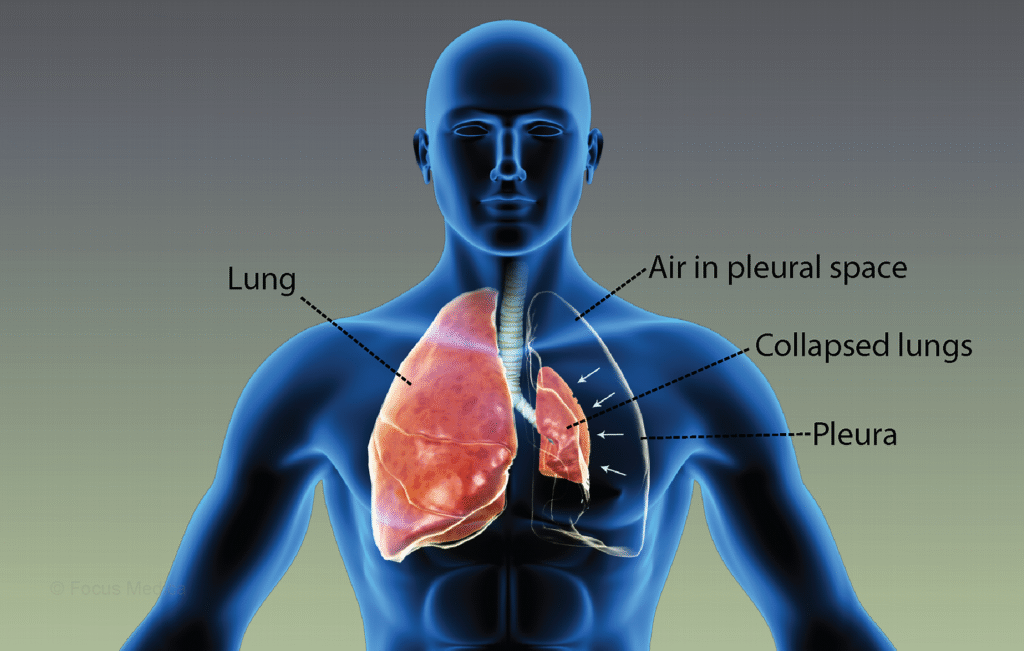
A collapsed lung, also known as a pneumothorax, occurs when air leaks into the space between the lung and chest wall, preventing the lung from expanding properly when you breathe.
- Primary spontaneous pneumothorax occurs in healthy individuals due to small air blisters (blebs) bursting.
- Secondary spontaneous pneumothorax – happens in people with existing lung conditions like COPD, tuberculosis, or lung cancer.
- Trauma – caused by chest injuries from accidents, medical procedures, or even acupuncture.
- Environmental factors – smoking, vaping, and air pollution can increase the risk.
Signs and Symptoms
- Sudden, sharp chest pain
- Shortness of breath
- Increased heart rate
- Pain that worsens when breathing in.
Treatment
- Small pneumothorax may heal on its own without treatment.
- Larger pneumothorax – may require a needle or chest tube to remove trapped air.
- Severe cases – emergency treatment is needed if the lung collapse affects other organs.
If you or someone you know experiences sudden chest pain and difficulty breathing, call 999/112 for emergency help.
Sucking Chest Wound
A sucking chest wound is a serious medical emergency that occurs when an injury creates an opening in the chest, allowing air to enter the chest cavity instead of the lungs2. This can lead to a collapsed lung (pneumothorax) and difficulty breathing.
Symptoms
- A visible hole in the chest
- A sucking or hissing sound when breathing
- Shortness of breath or rapid breathing
- Bright red or foamy blood around the wound
- Coughing up blood
- Bluish skin due to a lack of oxygen
Treatment
- Call 999/112 emergency services immediately – this is a life-threatening condition.
- Do not remove any objects stuck in the wound – this can worsen the injury.
- Seal the wound – use a sterile plastic covering or a chest seal, taping it down on three sides to allow air to escape but not enter.
- Monitor for signs of a collapsed lung – if symptoms worsen, remove the seal to relieve pressure.
- Keep the person as still as possible, minimising movement to prevent further injury. Tilt slightly to the wounded side; this will allow blood to drain.
- If they lose consciousness, perform CPR – if trained to do so.

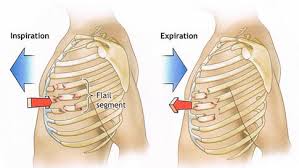
Flail Chest
Flail chest is a serious medical condition that occurs when multiple adjacent ribs are broken in multiple places, causing a segment of the chest wall to move independently from the rest of the rib cage. This results in paradoxical breathing, where the flail segment moves in the opposite direction to the rest of the chest wall during respiration.
Symptoms
- Chest pain and shortness of breath.
- Shallow breathing due to extreme pain.
- Hypoxia (lack of oxygen), which may cause lips or fingers to turn blue.
Causes
- Trauma, such as motor vehicle accidents or falls, is especially common in older individuals with osteoporosis.
- Blast injuries or crush injuries.
Treatment
- Oxygen therapy and pain management are used to stabilise breathing.
- Surgical intervention may be required to fix the fractures and improve outcomes.
- Non-invasive positive pressure ventilation can help support breathing.
Flail chest is often accompanied by pulmonary contusion, a bruise of the lung tissue that can interfere with blood oxygenation. If you or someone you know experiences symptoms after trauma, seek immediate medical attention.